Information on Hormone Imbalances Treated
Dr Jonathan Katz has experience in managing many hormone disorders, including, but not limited to:
- Overactive thyroid (thyrotoxicosis)
- Underactive thyroid (hypothyroidism)
- Thyroid enlargement / goitre
- Polycystic ovary syndrome
- Diabetes- Type 1, Type 2 diabetes and diabetes prevention
- Pituitary disease (e.g.prolactinomas, pituitary tumours)
- Testosterone deficiency
- Addison’s disease (and adrenal disorders)
Thyroid Disorders
Overactive (thyrotoxic) patients may experience one or more of a range of symptoms including sweating, weight loss, a feeling of excessive heat, palpitations, mood changes and insomnia. Occasionally patients have no symptoms and an abnormality is found on a blood test to suggest an overactive thyroid
Under active (hypothyroid) patients may experience one or more of a range of symptoms including fatigue, weight gain, feeling cold, dry skin, hair falling out. These symptoms can also occur without any thyroid hormone imbalance.
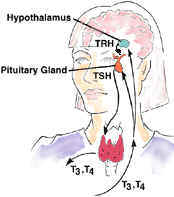
In normal health, thyroid hormone production is monitored and kept in balance by the brain. If the brain detects low levels of thyroid hormone, it increases production of 2 hormones – TRH and thereby TSH – to stimulate the thyroid. Thyroid stimulating hormone (TSH) comes from the pituitary and its levels are decreased when the thyroid is overactive and increased when the thyroid is under active, in an effort to normalise the levels of thyroid hormone in the blood.
Patients with an overactive thyroid (thyrotoxicosis) have raised thyroid hormone levels (high free T3 or free T4) which suppress the output of TSH from the pituitary (giving a low TSH on a blood test). This may be caused by certain drugs, by a viral infection (transient), the immune system (autoimmune disease) or by a “hot nodule” within the thyroid gland.
Patients with an under active thyroid (hypothyroidism) usually have low levels of thyroid hormone (fT4) and high levels of TSH in the blood. This is usually caused by the immune system turning on the thyroid and destroying cells in the thyroid (autoimmune disease).
Both thyrotoxicosis and hypothyroidism can be treated with medication to either decrease or increase thyroid hormone levels respectively, resulting in thyroid hormone levels in the normal range. The duration of treatment depends on the condition and this can be discussed further at your consultation.
For more information on thyroid disorders, visit the British Thyroid Foundation website at: http://www.btf-thyroid.org/
Polycystic Ovary Syndrome

Polycystic Ovary Syndrome (PCOS) is a common condition affecting 5% of women. PCOS may cause a range of symptoms – irregular periods or no periods at all; unwanted hair growth (hirsutism) on the face, chest or stomach; thinning of hair on top of the head; acne or spots; greasy skin. The syndrome is defined by one or more of these symptoms combined with either a “polycystic ovary” appearance on ultrasound, such as the picture above or a blood test showing higher levels of testosterone in the blood than in other women (all women have some testosterone in the blood). Treatment can range from diet and lifestyle advice (particularly if you are overweight) to cosmetic treatment (via your beautician) and , finally, medication. There are many possible avenues to explore and I would recommend a treatment plan, tailored to your particular symptoms and circumstances.
For more information on PCOS , visit the website of the PCOS patient support group, Verity: http://www.verity-pcos.org.uk/
Pituitary Disorders
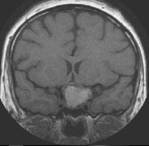
This is a picture of a rare pituitary tumour (craniopharyngioma) but most pituitary tumours are smaller than this. The commonest tumour we see is a prolactinoma, usually less than the size of a pea and these almost always respond to treatment with medication. Occasionally, we see larger tumours such as the one above, which require neurosurgery to remove them. Patients who have had pituitary tumours, neurosurgery or cranial irradiation usually require follow-up checks to ensure they do not have one or more pituitary hormone deficiencies.
For more information on pituitary disorders and patient support groups, contact the Pituitary Foundation: http://www.pituitary.org.uk/
Diabetes

The number of people affected by both Type 1 (Type1DM) and Type 2 Diabetes (Type 2DM) in the UK, and other developed countries, is increasing fast. The biggest increase has been seen in the development of Type 2 Diabetes which is largely a result of increasing levels of weight problems and decreased physical activity. Type 2DM used to be diagnosed mainly in older patients but now we see this condition arising in patients as young as 20 years old (sometimes younger).
Weight gain, particularly around the middle (central obesity) is a key factor. Type 2 DM is usually initially best treated with diet and exercise. Later tablets will be required. If the diet and tablets fail to control the diabetes, injectable treatment with incretins or insulin will follow. Type 1DM on the other hand is treated with insulin from the start.
The aim of treatment in both Type1DM and Type2DM is to achieve good blood sugar control and control the cardiovascular risk factors – smoking, blood pressure, cholesterol – to minimise the risks of developing complications of diabetes and, when these occur, to slow or limit the progression of complications.
Potential complications include diabetic eye disease (retinopathy), kidney disease (nephropathy), foot complications (neuropathy or poor circulation) , heart attack or stroke. Some patients develop no complications, but with time most will develop one or more: